Behind the COVID-19 Diagnostic for Testing Hundreds of People at a Time
This is the story of the scientists working towards clinical application and the research that started long before the pandemic.
“I never thought we’d be doing this in the midst of a pandemic.”
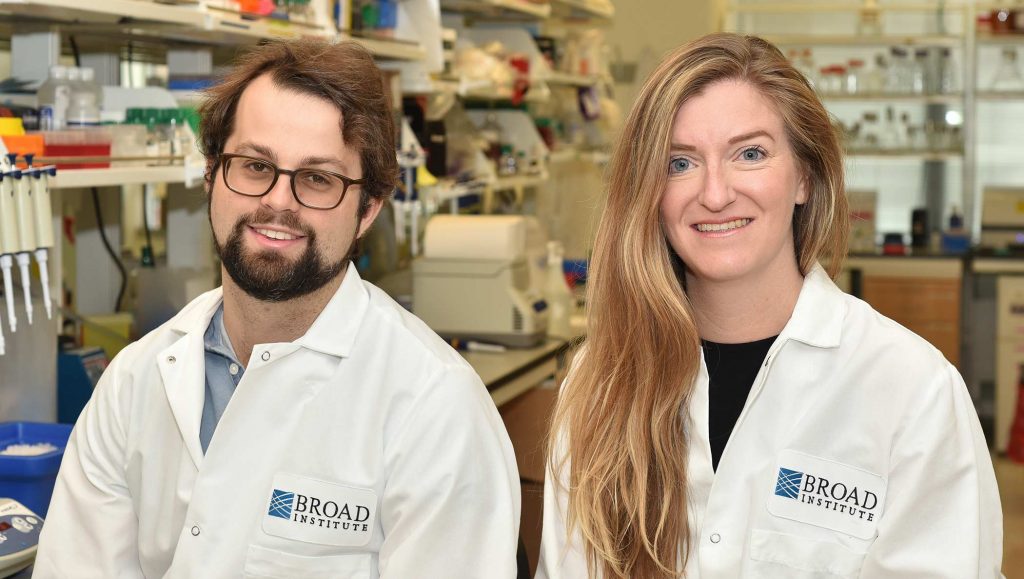
Since high school, Dr. Cameron Myhrvold has been in the laboratory, first studying insect flight and later, as a graduate student and Hertz Fellow, studying bacterial communication.
Now he’s focused on applying the award-winning technology he developed previously to large-scale testing for COVID-19. He calmly describes how this came to be, every once in a while leaning forward with excitement as he recalls a breakthrough.
The technology is called CARMEN, which stands for Combinatorial Arrayed Reactions for Multiplexed Evaluation of Nucleic acids, and it can be used to test many individuals for many different viruses at the same time. After developing the initial CARMEN technology with fellow Hertz Fellowship recipient Dr. Cheri Ackerman, Cameron’s role in the transition of CARMEN for COVID-19 testing has taken place largely away from the lab bench.
Focusing on viruses—before one caused a global pandemic
“It’s so amazing something so tiny with a couple of genes can have such a big effect on human health,” says Cameron. Even over Zoom, his face clearly lights up as he describes how he first became interested in viruses.
Despite the current global focus on SARS-CoV-2, the coronavirus that causes COVID-19, science has not always paid as much attention to viral outbreaks.
“Growing up there were some outbreaks, [they were] something that people were vaguely aware of," says Cameron. Later he began to notice a trend in which there was a major outbreak every few years. First it was H1N1, a type of flu virus; followed by Ebola, a deadly virus that involves internal or external bleeding; and then by Zika, a virus spread by mosquitos.
“This trend,” Cameron says, “that’s what motivated me. I wanted to take my background from my PhD to go after this important problem related to viruses and outbreaks.”
Learning science by doing science
Cameron says that being homeschooled “allowed me to try doing science more than just learning about it.” During high school, he spent his summers at the University of Washington using high speed video to understand how insects control their flight. “This got me really hooked on doing science,” he says.
Talking quickly, as if telling a story that happened just yesterday, he describes how his enthusiasm for science continued during his undergraduate studies at Princeton. “It was my first time really doing molecular biology,” he says of his time there studying how bacteria cells communicate with each other as they grow.
“It was hard,” says Cameron, “but I wanted to get better at it.” He continued learning by doing science during his PhD at Harvard Medical School. Supported by a Hertz Fellowship, he began to use nanotechnology to develop a variety of research tools, some of which he used to study bacteria.
Choosing topics where the most impact can be made
“[It] felt to me that the problem we were going after was something that other people were not focusing on as much,” says Cameron. He appears thoughtful as he considers what motivated him to try to develop better testing for infectious diseases when he joined the Sabeti Lab after earning his PhD.
Cameron was interested in using a newly discovered CRISPR (clustered regularly interspaced short palindromic repeats) system called Cas13. A CRISPR system is like a pair of scissors that can be used to cut genetic material.
He said the team came together naturally due to a mutual excitement about the still-new application of CRISPR to infectious disease testing. At the start, Cameron was joined by Catherine Freije, a graduate student in the Sabeti Lab at the time, and collaborators at Massachusetts Institute of Technology, Jonathan Gootenberg and Omar Abudayyeh.
Together, they used the “CRISPR scissors” to recognize specific viruses, something that had been done with other CRISPR systems but not yet with Cas13. If an individual is infected, the scissors cut up indicators, which create a light-based signal that is read as a positive test result.
The potential impact of using Cas13 for infectious disease testing and treatment landed Cameron and Catherine a spot on the Forbes 30 Under 30 Healthcare list in 2019. Hoping to realize that impact, the team worked to increase the number of individual samples that could be read with one test, expanding to include members of the Blainey Lab. The result was CARMEN.
Initially, Cameron says that using CARMEN in a clinical setting was “something that we were shooting for because there is this unmet need in terms of being able to test lots of different samples for lots of different viruses.” But the opportunity to apply CARMEN came a lot sooner than planned with the need for increased testing during the COVID-19 pandemic.
Accelerating to meet COVID-19 testing demands
“I love a challenge.”
Nicole Welch is the Sabeti Lab graduate student who led the early in-laboratory effort to adapt CARMEN for COVID-19 testing. Building on the first version of CARMEN, the diagnostic test uses nasal swabs from up to 180 individuals and tests each individual for nine common viruses that affect the lungs, including COVID-19. “It’s refreshing to be working on something that could have an impact on the community in a matter of months,” says Nicole.
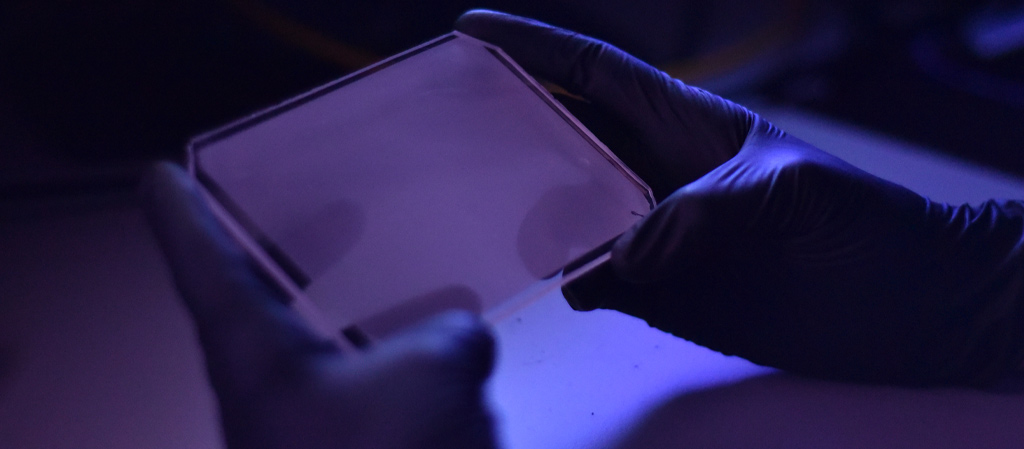
At the start of the pandemic, Nicole set aside her other work and took on the project full time. She describes being mostly alone in a normally bustling lab, setting up CARMEN tests and connecting with Cameron and the rest of the team over Zoom. Nearby in the Blainey Lab, visiting master’s student Juliane Weller and others were working on test readout and data analysis.
Wide-eyed and adamant, Nicole says she did not expect to be taking the project all the way to potential clinical application. She laughs as she considers how quickly they have been able to get CARMEN ready despite working during the pandemic. “There have been a few moments where Cameron and I message each other on the side during a big meeting to stay on after,” says Nicole, explaining how the two would stay on Zoom after others had left to take in the excitement surrounding the work together.
Nicole and Cameron continue to rapidly develop CARMEN for COVID-19 testing, with Nicole still primarily in the lab and Cameron leading remotely. However, they emphasize that this has been a major team effort. They are joined by additional collaborators in the Sabeti Lab and the Blainey Lab at the Broad Institute, as well as clinical laboratory collaborators at Massachusetts General Hospital.
Measuring success in knowledge gained, shared, and applied
“I do see a path forward here,” says Cameron, “and I am very excited about the future of this.”
At the beginning of 2021, Cameron established the Myhrvold Lab at Princeton University in the Department of Molecular Biology. He plans for the lab to “continue building on the success we’ve had using Cas13-based technology for detecting and destroying viruses,” in addition to “developing other technologies to study RNA more broadly.” For his previous work with Cas13, Cameron was named a 2020 STAT Wunderkind, an award given to early-career scientists for their impact on the life sciences.
Instead of focusing on scientific awards, Cameron has always measured his success in new knowledge gained and shared. Looking forward, he excitedly describes what he’s calling a “broadening of my scientific horizons.” He explains that while there is still “compelling and important work to do with impact on human health,” he hopes to shift his focus to a “broader application of technology for his [scientific] colleagues.”
“The reason we developed a lot of the things we developed is to have them used by other people,” says Cameron. “Seeing it actually get out there is very rewarding.”
About the Author: Sarah D. Slack is currently a research associate in the Sabeti Lab at the Broad Institute developing antiviral therapies for RNA viruses using CRISPR-Cas13. She completed this piece as part of a course in Boston University’s online Health Communication graduate program.